Translational Research
From Bench to Bedside and Back Again in Pediatric Brain Injury
 Susan Margulies and her colleagues used to study a brain or lung injury in vivo in the lab and only record what happened. If an animal stopped breathing, they observed. If its blood pressure fell, they waited. But clinicians who are integral members of Margulies’s research teams have changed all that.
Susan Margulies and her colleagues used to study a brain or lung injury in vivo in the lab and only record what happened. If an animal stopped breathing, they observed. If its blood pressure fell, they waited. But clinicians who are integral members of Margulies’s research teams have changed all that.
Clinicians in pediatrics, critical care medicine, anesthesia, pulmonary medicine, neurosurgery and neonatology routinely identify important research areas and clinically relevant questions for the Margulies lab to pursue. Their participation in research design has fundamentally changed experimental designs and protocols by including clinically relevant practices. “We have moved from passive observation of the cascade of events that often occur after an injury to the brain,” says Margulies,”to more active management that mimics the clinical setting.”
One of Margulies’s areas of study—traumatic brain injury in children—is a high-priority topic.”Traumatic brain injury (TBI) is the leading cause of death and acquired disability in childhood in the United States,” Margulies wrote recently. “Every year, more than 200,000 children in the U.S. suffer traumatic brain injuries. By midnight tonight, nearly thirty children will have died from injuries incurred today, several times that number will develop lifelong disability, and even more will exhibit at least transient impairment of learning, development, and behavior.”
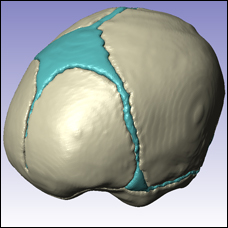
 “Despite this tragically high incidence and its enormous cost, there are no specific treatments for traumatic brain injuries in children,” Margulies points out. To understand how to treat TBI in children, Margulies and her colleagues are studying piglets which closely resemble the human infant and toddler in brain development. For more than 10 years, they have developed and tested these models for TBI research specifically with relevance to children.
“Despite this tragically high incidence and its enormous cost, there are no specific treatments for traumatic brain injuries in children,” Margulies points out. To understand how to treat TBI in children, Margulies and her colleagues are studying piglets which closely resemble the human infant and toddler in brain development. For more than 10 years, they have developed and tested these models for TBI research specifically with relevance to children.
To keep mutually informed, Journal Club meets every week to discuss the literature in pediatric head injury. Sometimes the paper is very clinical, says Margulies, sometimes very technical; sometimes a new paper, and sometimes a classic. “In the highly charged arena—socio-, medical, legal arena—of child abuse, it’s as important for a clinician to understand biomedical advances as for engineers to understand new clinical findings,” she explains. When they discuss computational model papers, clinicians learn how assumptions about material properties can influence predictions, she says—”garbage in, garbage out. When we discuss clinical papers,” she continues,”engineers learn about treatment trials for brain injury. [This] provides motivation for research in prevention and understanding injury mechanisms, so we can improve detection and management.”
 These extensive collaborations have enriched Margulies’ research and that of her students. Collaboration “is constant and pervasive throughout all” the lab does, says Margulies. “Most of my students have clinicians on their PhD committee, and I have been a primary research mentor for about a dozen clinicians.” Residents bring bioengineering graduate students into the hospital to see TBI patients first-hand. “Cross-disciplinary training is really important,” says Margulies. “I believe in it.” One day soon, she hopes, their multidisciplinary pre-clinical studies will help to identify agents ready for rapid translation to clinical trials for the treatment of pediatric traumatic brain injury.
These extensive collaborations have enriched Margulies’ research and that of her students. Collaboration “is constant and pervasive throughout all” the lab does, says Margulies. “Most of my students have clinicians on their PhD committee, and I have been a primary research mentor for about a dozen clinicians.” Residents bring bioengineering graduate students into the hospital to see TBI patients first-hand. “Cross-disciplinary training is really important,” says Margulies. “I believe in it.” One day soon, she hopes, their multidisciplinary pre-clinical studies will help to identify agents ready for rapid translation to clinical trials for the treatment of pediatric traumatic brain injury.